
Overcoming Barriers to Medication Access
Patients who do not take medications as prescribed cost the healthcare system up to $289 billion annually. However, there’s more to the story than people just skipping doses or forgetting
Health Advocate Named Great Place to Work for 2023
Health Advocate has once again been certified as a Great Place To Work®.
Health Advocate Earns NCQA Certification for HEDIS® Certified Measures
Health Advocate announced today that its Health Insights Dashboard™ has received the National Committee for Quality Assurance (NCQA) Measure Certification™ for the Healthcare Effectiveness Data and Information Set (HEDIS) measures for the seventh
Supporting Mental Health in the Workplace | Health Advocate’s Ask the Expert Series
May is Mental Health Awareness Month, a great opportunity to talk about what is top of mind right now when it comes to supporting employees’ mental health and well-being.
Health Advocate Taps Industry Expert Alyssa Scott, PhD, to Lead Next Generation Analytics Products and Services
Health Advocate announced today that Alyssa Scott has joined the organization as Senior Vice President, Healthcare Analytics, leading the organization's Engagement Analytics division.
‘I got a colonoscopy at 28’
Colorectal cancer rates in people under 55 are rising according to a new report from the American Cancer Society.
Health Advocate Recognized for Excellence in Service by National Customer Service Association
Health Advocate announced today that it has been selected as Service Organization of the Year in the 2023 National Customer Service Association (NCSA) Service All-Star Awards.
Compassionate Support During a Difficult Time
When Jason Boone’s car was hit by a drunk driver in 2021, the former pro-athlete was unsure how to begin navigating next steps, so he reached out to Health Advocate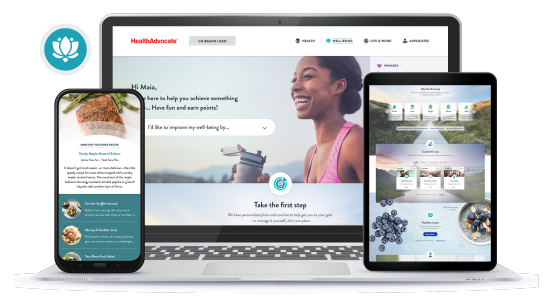
Health Advocate Launches Reimagined Be True Well-Being Program
Health Advocate announced today the launch of its all-new Be True Well-Being program, a total well-being experience.

